Dementia Prevention: Exploring The Potential Protective Effects Of The Shingles Vaccine

Table of Contents
The Link Between Herpes Zoster Virus (HZV) and Dementia
The herpes zoster virus (HZV), responsible for chickenpox and its reactivation as shingles, has increasingly been implicated in cognitive decline and dementia risk. The connection isn't direct, but rather involves a complex interplay of inflammation and neuronal damage.
- HZV reactivation (shingles) is linked to inflammation in the brain: The inflammatory response triggered by HZV reactivation can extend beyond the skin, affecting the nervous system and potentially contributing to neurodegeneration.
- Chronic inflammation is a known risk factor for various neurodegenerative diseases, including Alzheimer's disease: Persistent inflammation in the brain disrupts normal cellular function and accelerates the progression of neurodegenerative processes.
- Studies suggest that HZV may contribute to the development of neurofibrillary tangles and amyloid plaques – hallmarks of Alzheimer's: These abnormal protein structures are characteristic of Alzheimer's disease, and research hints at a possible role for HZV in their formation or exacerbation.
- Latent HZV can reactivate and contribute to cognitive decline: Even after a chickenpox infection, the virus can remain dormant in nerve cells, potentially reactivating later in life and contributing to chronic inflammation and cognitive impairment. This latent infection could be a significant underlying factor impacting dementia risk.
The Shingles Vaccine: A Potential Protective Mechanism
The shingles vaccines, Zostavax and the newer Shingrix, are designed to prevent shingles by stimulating the immune system to fight against HZV. This prevention may have broader implications for brain health.
- The vaccine reduces the incidence of shingles and its associated complications: By preventing HZV reactivation, the vaccine directly addresses one potential pathway leading to neuroinflammation.
- By preventing HZV reactivation, the vaccine may reduce chronic inflammation in the brain: This reduction in inflammation is a key potential mechanism for the observed association with reduced dementia risk.
- Shingrix, a newer recombinant subunit vaccine, offers higher efficacy and longer-lasting protection compared to Zostavax: This makes Shingrix a potentially more impactful tool in dementia prevention strategies.
- Several observational studies have shown a correlation between shingles vaccine uptake and reduced dementia incidence: While these studies don't prove causation, they suggest a potential link that warrants further investigation. These studies have fuelled interest in larger, more definitive trials.
Mechanisms of Potential Protection
The protective effect of the shingles vaccine against dementia may stem from several biological mechanisms:
- Reduction of systemic inflammation: Preventing shingles reduces a significant source of inflammation, potentially lessening the overall inflammatory burden on the body, including the brain.
- Improved immune response to other pathogens: A robust immune response, stimulated by the vaccine, may offer broader protection against other infections that could contribute to cognitive decline.
- Prevention of neuronal damage caused by HZV: By preventing HZV reactivation, the vaccine directly prevents neuronal damage caused by viral replication and the resulting inflammatory response.
Current Research and Future Directions
The relationship between the shingles vaccine and dementia risk remains an active area of research.
- Several ongoing clinical trials are investigating this link more rigorously: These larger-scale studies are crucial for confirming the findings from observational studies and establishing a clearer understanding of cause and effect.
- Larger-scale, randomized controlled trials are needed to confirm the findings: Observational studies can demonstrate correlation, but only randomized controlled trials can definitively prove causation.
- Limitations of current research include the reliance on observational studies and the challenges in isolating the effects of the vaccine from other contributing factors: Confounding variables related to lifestyle, genetics, and other health conditions need to be carefully considered.
- Establishing a direct causal relationship between the shingles vaccine and dementia prevention requires more extensive research: The complexity of neurodegenerative diseases necessitates further investigation to understand the precise mechanisms involved.
Practical Implications and Considerations
The potential protective effects of the shingles vaccine against dementia raise significant implications for public health:
- Whether the shingles vaccine should be recommended as a strategy for dementia prevention requires careful consideration: While the evidence is promising, more research is needed before widespread recommendation for this specific purpose.
- Age-related factors and vaccine efficacy need to be considered: Vaccine effectiveness can vary with age, and the risk of dementia increases with age.
- Cost-effectiveness and accessibility of the vaccine are crucial factors: Widespread adoption depends on affordability and equitable access to the vaccine.
- Consulting with healthcare professionals is vital for personalized recommendations: Individual risk factors and health conditions should be assessed before making decisions about vaccination.
Conclusion
Emerging evidence suggests a potential link between the shingles vaccine and a reduced risk of dementia. While further research is crucial to definitively establish a causal relationship, the existing data warrants further investigation into the protective mechanisms and potential benefits of the shingles vaccine in dementia prevention. This could represent a significant advancement in safeguarding cognitive health and reducing the burden of this devastating disease.
Call to Action: Consult your doctor to discuss your risk factors for shingles and dementia, and inquire about the suitability of the shingles vaccine for your individual needs. Protecting your brain health through proactive measures like the shingles vaccine may be a crucial step in dementia prevention.

Featured Posts
-
 Multiple Studies Link Shingles Vaccination To Lowered Dementia Risk
Apr 25, 2025
Multiple Studies Link Shingles Vaccination To Lowered Dementia Risk
Apr 25, 2025 -
 127 Years Of Brewing History Anchor Brewing Companys Closure
Apr 25, 2025
127 Years Of Brewing History Anchor Brewing Companys Closure
Apr 25, 2025 -
 Palisades Fires Which Celebrities Lost Their Homes A Comprehensive List
Apr 25, 2025
Palisades Fires Which Celebrities Lost Their Homes A Comprehensive List
Apr 25, 2025 -
 How Trumps Presidency Will Impact Mark Zuckerberg And Meta
Apr 25, 2025
How Trumps Presidency Will Impact Mark Zuckerberg And Meta
Apr 25, 2025 -
 Analyzing The Decline Of Bmw And Porsche Sales In China Causes And Solutions
Apr 25, 2025
Analyzing The Decline Of Bmw And Porsche Sales In China Causes And Solutions
Apr 25, 2025
Latest Posts
-
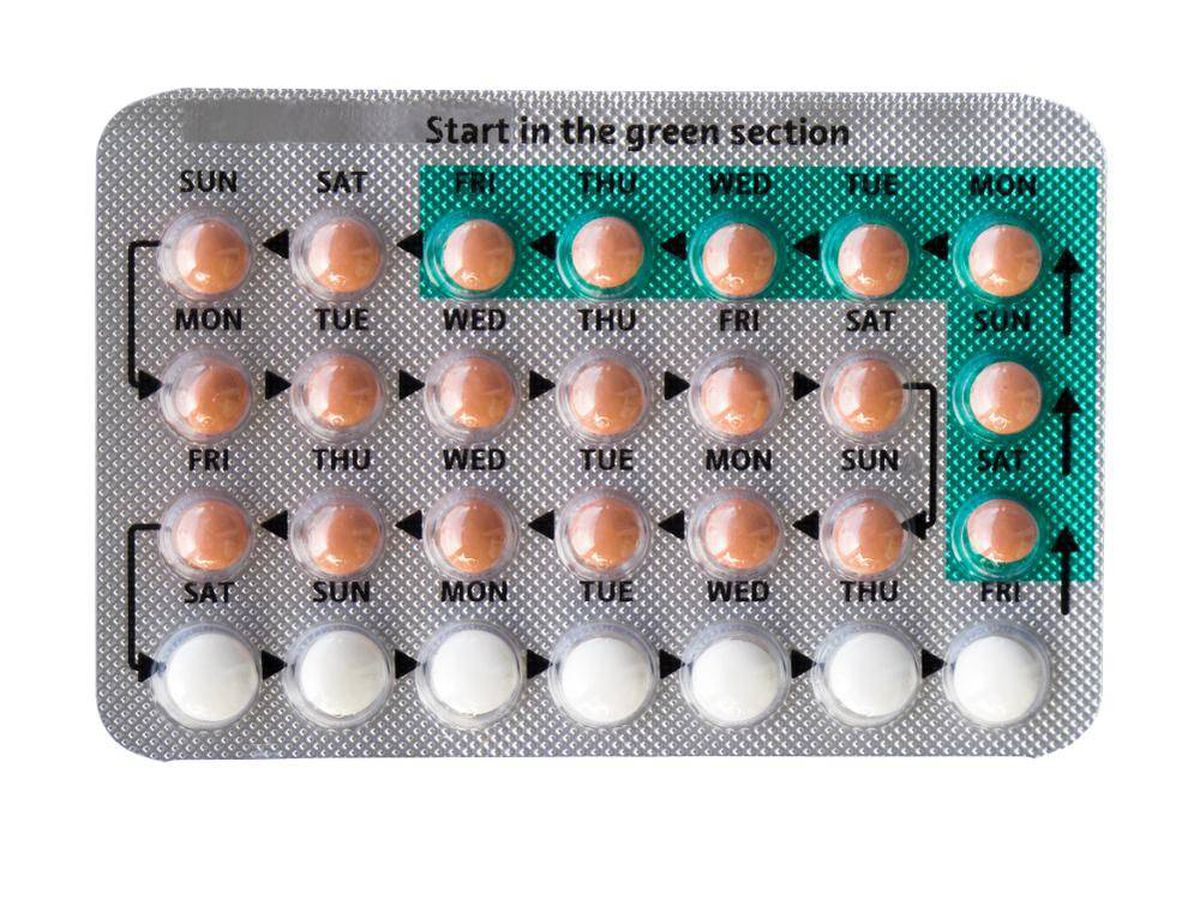 The Rise Of Otc Birth Control A Post Roe Analysis
Apr 25, 2025
The Rise Of Otc Birth Control A Post Roe Analysis
Apr 25, 2025 -
 Over The Counter Birth Control Implications For Reproductive Rights After Roe V Wade
Apr 25, 2025
Over The Counter Birth Control Implications For Reproductive Rights After Roe V Wade
Apr 25, 2025 -
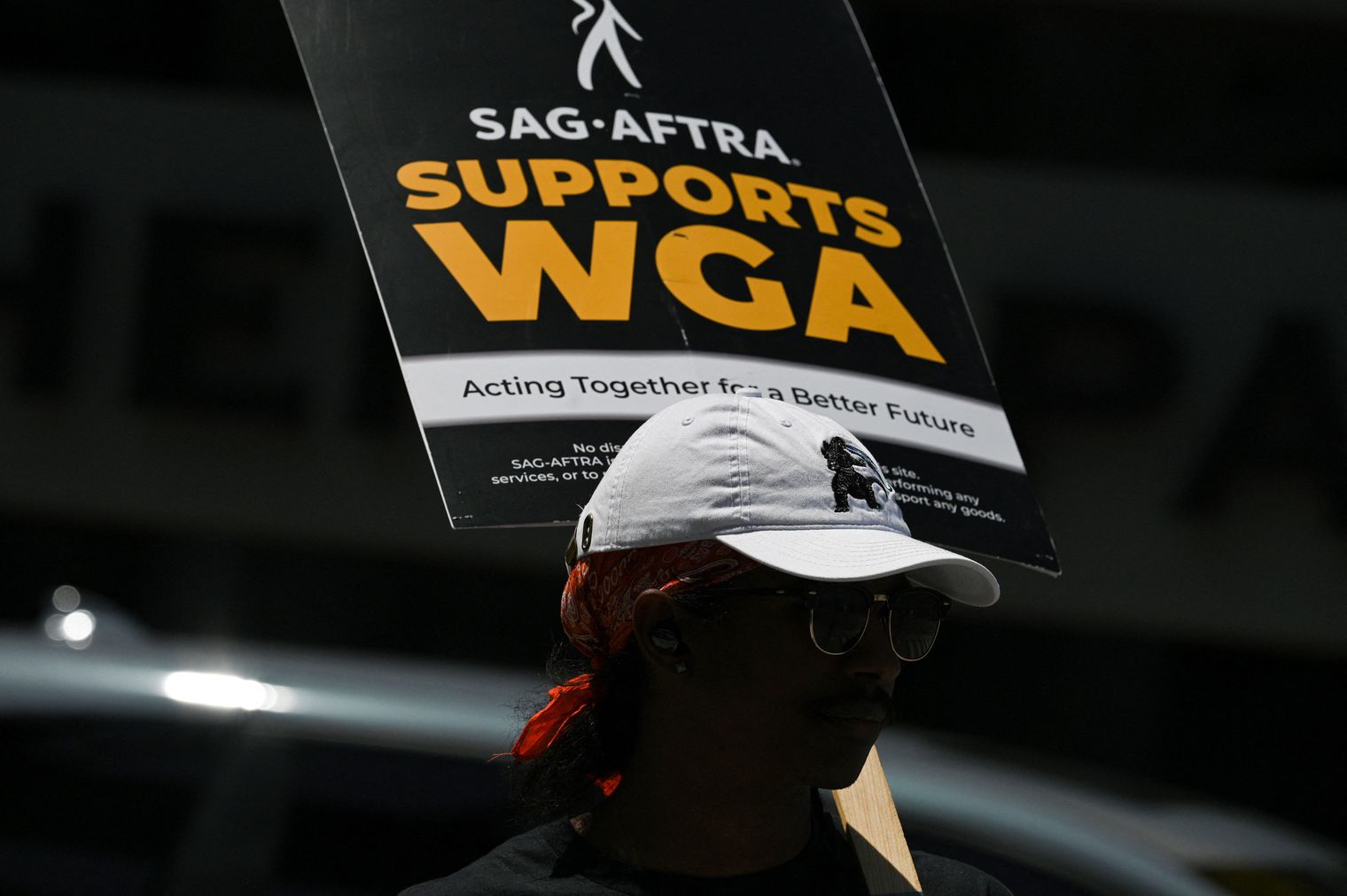 Hollywood Production Grinds To Halt As Sag Aftra Joins Wga On Strike
Apr 25, 2025
Hollywood Production Grinds To Halt As Sag Aftra Joins Wga On Strike
Apr 25, 2025 -
 Post Roe America How Otc Birth Control Is Reshaping Reproductive Healthcare
Apr 25, 2025
Post Roe America How Otc Birth Control Is Reshaping Reproductive Healthcare
Apr 25, 2025 -
 Hollywood Shut Down Writers And Actors Strike Impacts Film And Television
Apr 25, 2025
Hollywood Shut Down Writers And Actors Strike Impacts Film And Television
Apr 25, 2025
