Mental Health Care Reform: Prioritizing Patient Access And Quality
Table of Contents
Addressing Barriers to Access
Many factors prevent individuals from receiving the mental healthcare they need. These barriers can be broadly categorized as financial, geographic, and systemic. Overcoming these obstacles is paramount to achieving meaningful mental health care reform.
Financial Barriers
High costs of treatment, lack of insurance coverage, and inadequate reimbursement rates for providers significantly impact access to care. Many individuals, particularly those from low-income backgrounds, face insurmountable financial hurdles.
- The Affordable Care Act (ACA) and Mental Health Coverage: While the ACA expanded mental health coverage, significant gaps remain. Many plans still have high deductibles and co-pays, making treatment unaffordable for many.
- Increased Government Funding and Subsidies: Increased government investment in mental healthcare is crucial to ensuring affordability. This includes subsidies for individuals and increased reimbursement rates for providers.
- The Role of Private Insurance Companies: Private insurance companies must play a larger role in expanding access by improving coverage, reducing out-of-pocket costs, and promoting parity between mental and physical healthcare benefits.
- Innovative Payment Models: Exploring and implementing innovative payment models, such as value-based care and telehealth reimbursement models, can improve affordability and incentivize quality care.
Geographic Barriers
The availability of mental health professionals is unevenly distributed, with significant shortages in rural and underserved areas. This creates substantial access challenges for individuals in these communities.
- Telehealth: Bridging the Geographic Divide: Telehealth offers a powerful solution, allowing individuals in remote areas to access mental health services remotely. This includes video conferencing, online therapy, and remote patient monitoring.
- Mobile Mental Health Units and Outreach Programs: Mobile units and outreach programs can bring services directly to those in need, overcoming transportation barriers and reaching underserved populations.
- Recruiting and Retaining Professionals in Underserved Areas: Incentivizing mental health professionals to work in underserved areas through loan forgiveness programs, higher salaries, and improved working conditions is vital.
- Training Community Health Workers: Training community health workers to provide basic mental healthcare can significantly expand access to care in underserved communities.
Systemic Barriers
Beyond financial and geographic limitations, systemic barriers such as stigma, long wait times, complex referral processes, and a lack of culturally competent care hinder access to mental healthcare.
- Combating Stigma through Public Awareness Campaigns: Public education campaigns are crucial to reducing the stigma surrounding mental illness and encouraging help-seeking behaviors.
- Streamlining Referral Processes and Appointment Scheduling: Simplifying referral processes and improving appointment scheduling systems can drastically reduce wait times and make accessing care more convenient.
- Culturally Sensitive and Linguistically Appropriate Services: Providing culturally sensitive and linguistically appropriate services is essential to ensuring that all individuals feel comfortable seeking and receiving care.
- The Role of Patient Advocacy Groups: Patient advocacy groups play a vital role in advocating for improved access to mental healthcare and ensuring that the voices of individuals with mental health conditions are heard.
Improving the Quality of Mental Healthcare
Improving access is only one part of effective mental health care reform. Equally important is enhancing the quality of care provided.
Enhancing Provider Training and Support
Investing in comprehensive training programs for mental health professionals is critical. This includes emphasizing evidence-based practices, trauma-informed care, and culturally competent care.
- Ongoing Professional Development and Continuing Education: Ongoing training is essential to keep providers updated on the latest research and best practices.
- Peer Support and Supervision: Peer support and supervision can help to improve provider morale, reduce burnout, and enhance the quality of care.
- Mentorship Programs for New Professionals: Mentorship programs can help to support new professionals and ensure that they receive the guidance and support they need.
- Addressing Provider Burnout and Promoting Wellbeing: Addressing provider burnout is crucial to maintaining a high-quality workforce and ensuring the sustainability of the mental health system.
Integrating Mental and Physical Healthcare
A holistic approach to healthcare is essential. Integrating mental health services into primary care settings improves access and addresses co-occurring conditions.
- Co-locating Mental Health Professionals in Primary Care Clinics: Co-locating mental health professionals in primary care clinics increases convenience and facilitates early intervention.
- Integrated Care Models for Co-occurring Conditions: Integrated care models effectively address the complex needs of individuals with both mental and physical health conditions.
- Screening for Mental Health Issues in Primary Care: Routine screening for mental health issues in primary care settings can identify individuals who need help early on.
- Improved Communication and Coordination between Providers: Improved communication and coordination between mental health and primary care providers are crucial for seamless care.
Utilizing Technology to Enhance Care
Technology offers significant opportunities to improve access, track progress, and personalize treatment.
- Telehealth for Remote Monitoring and Therapy: Telehealth enables remote monitoring and therapy sessions, expanding access to care for individuals in remote areas or with mobility limitations.
- Mental Health Apps for Self-Management and Support: Mental health apps provide self-management tools, support groups, and educational resources.
- Data Privacy and Security in Digital Mental Health Platforms: Ensuring data privacy and security is paramount in digital mental health platforms.
- User-Friendly and Accessible Digital Tools: Digital tools must be designed to be user-friendly and accessible to all, regardless of technical skills or abilities.
Conclusion
Effective mental health care reform requires a comprehensive strategy addressing barriers to access and improving the quality of care. This involves tackling financial, geographic, and systemic challenges, investing in provider training, integrating mental and physical healthcare, and leveraging technology. By prioritizing patient access and quality, we can create a system where everyone has the opportunity to receive the mental healthcare they need. Let's continue advocating for meaningful mental healthcare reform and for improvements in mental health services to ensure a healthier future for all.
Featured Posts
-
 10 Year Old Girl Dies On Rugby Pitch A Community In Grief
May 03, 2025
10 Year Old Girl Dies On Rugby Pitch A Community In Grief
May 03, 2025 -
 Souness Condemns Manchester Uniteds Latest Transfer Move
May 03, 2025
Souness Condemns Manchester Uniteds Latest Transfer Move
May 03, 2025 -
 Where To Watch The Wizarding World Holiday Marathon On Syfy
May 03, 2025
Where To Watch The Wizarding World Holiday Marathon On Syfy
May 03, 2025 -
 Watch England Vs Spain Tv Channel Kick Off Time And Viewing Guide
May 03, 2025
Watch England Vs Spain Tv Channel Kick Off Time And Viewing Guide
May 03, 2025 -
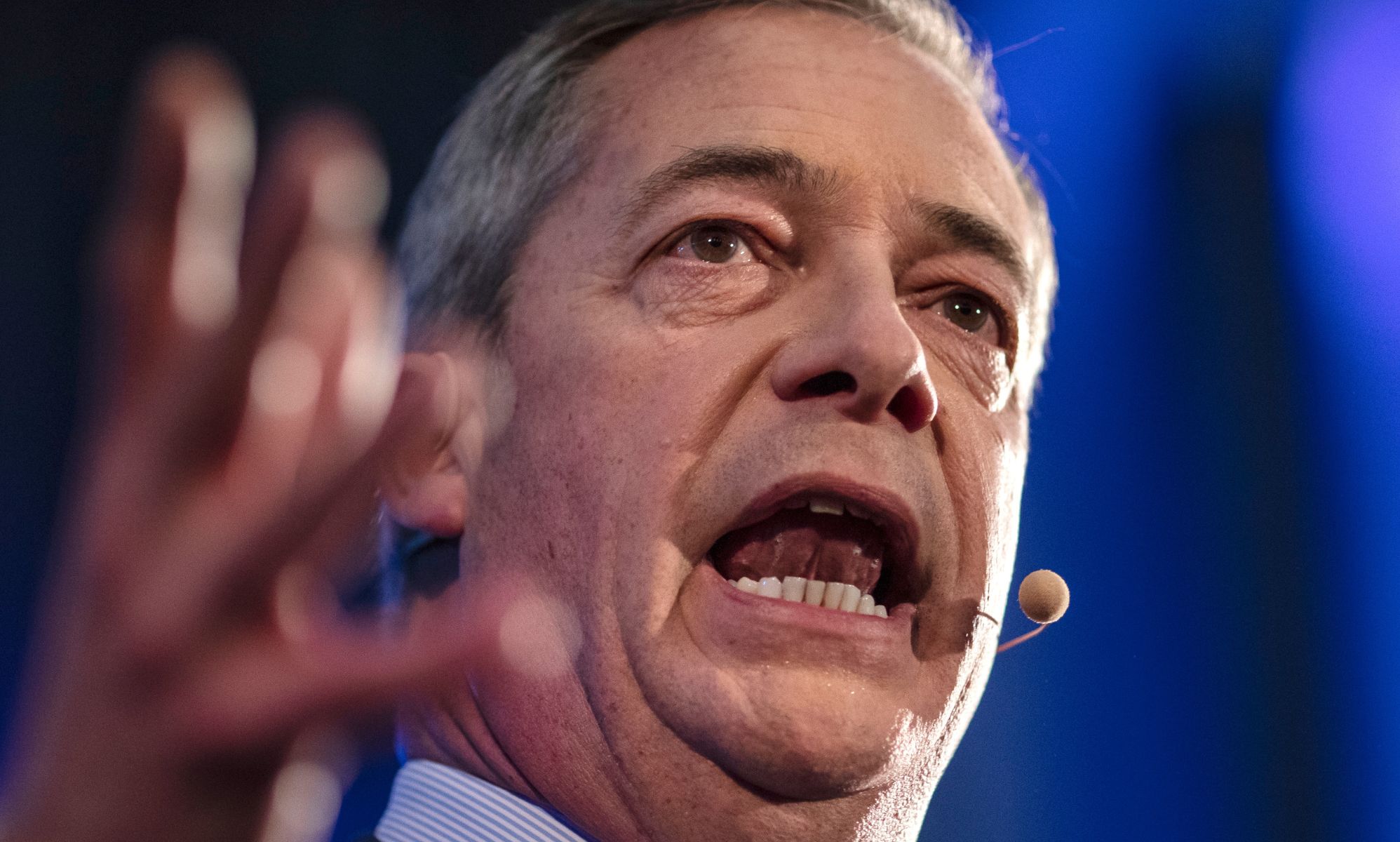 Nigel Farages Reform Uk Is Collapse Imminent Five Warning Signs
May 03, 2025
Nigel Farages Reform Uk Is Collapse Imminent Five Warning Signs
May 03, 2025
Latest Posts
-
 Affordable Housing In Strathdearn Tomatin Pupils Mark Groundbreaking Ceremony
May 04, 2025
Affordable Housing In Strathdearn Tomatin Pupils Mark Groundbreaking Ceremony
May 04, 2025 -
 Tomatins Strathdearn Gains Momentum Affordable Housing Project Begins
May 04, 2025
Tomatins Strathdearn Gains Momentum Affordable Housing Project Begins
May 04, 2025 -
 Netherlands Explores Ow Subsidy Revival To Stimulate Competition
May 04, 2025
Netherlands Explores Ow Subsidy Revival To Stimulate Competition
May 04, 2025 -
 Pupils Celebrate Groundbreaking Of New Affordable Homes In Tomatins Strathdearn
May 04, 2025
Pupils Celebrate Groundbreaking Of New Affordable Homes In Tomatins Strathdearn
May 04, 2025 -
 Will Renewed Ow Subsidies Encourage More Bids In The Netherlands
May 04, 2025
Will Renewed Ow Subsidies Encourage More Bids In The Netherlands
May 04, 2025
