Fungal Infections: A Growing Threat Of Antibiotic Resistance
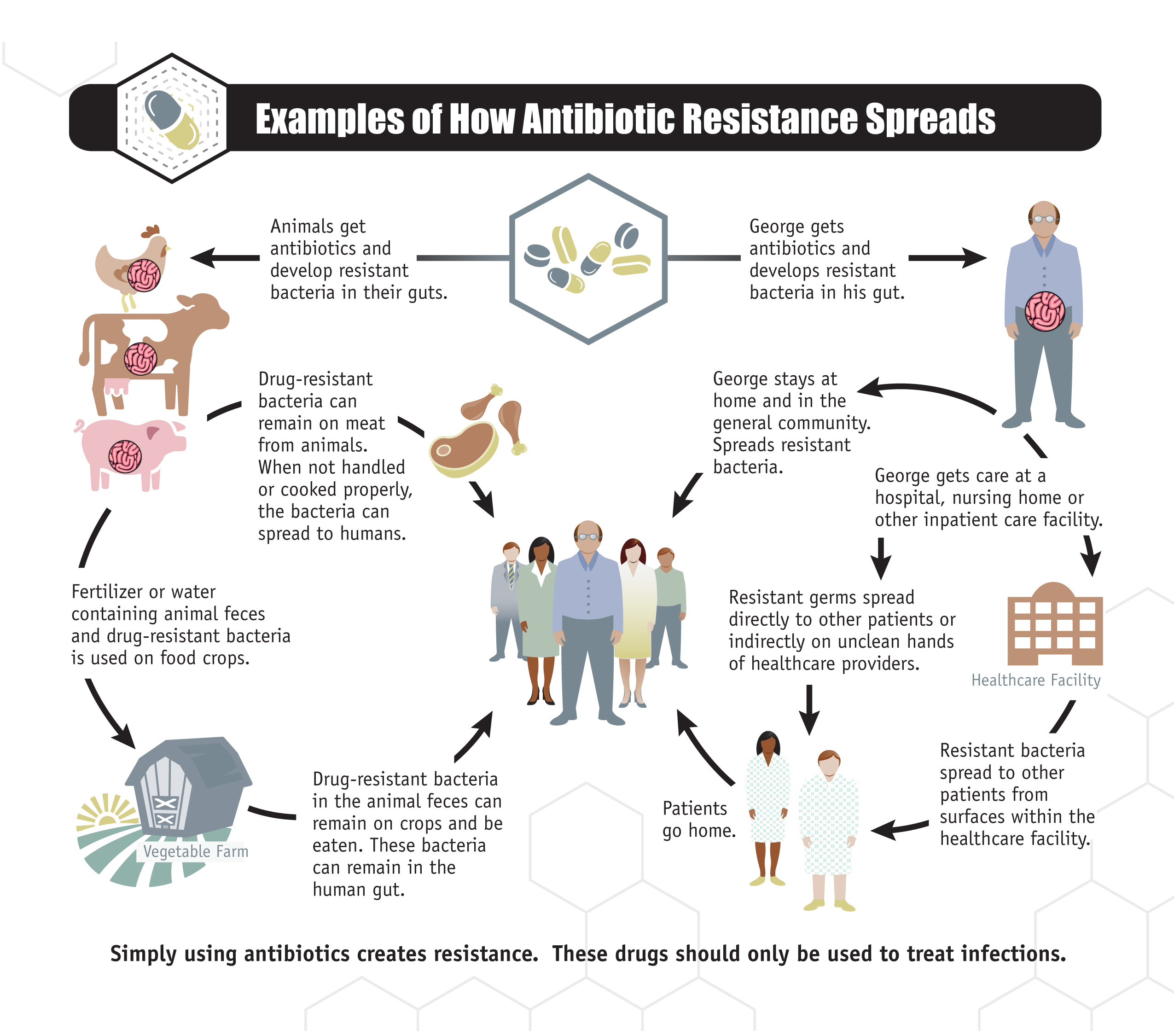
Table of Contents
The Rise of Antifungal Resistance
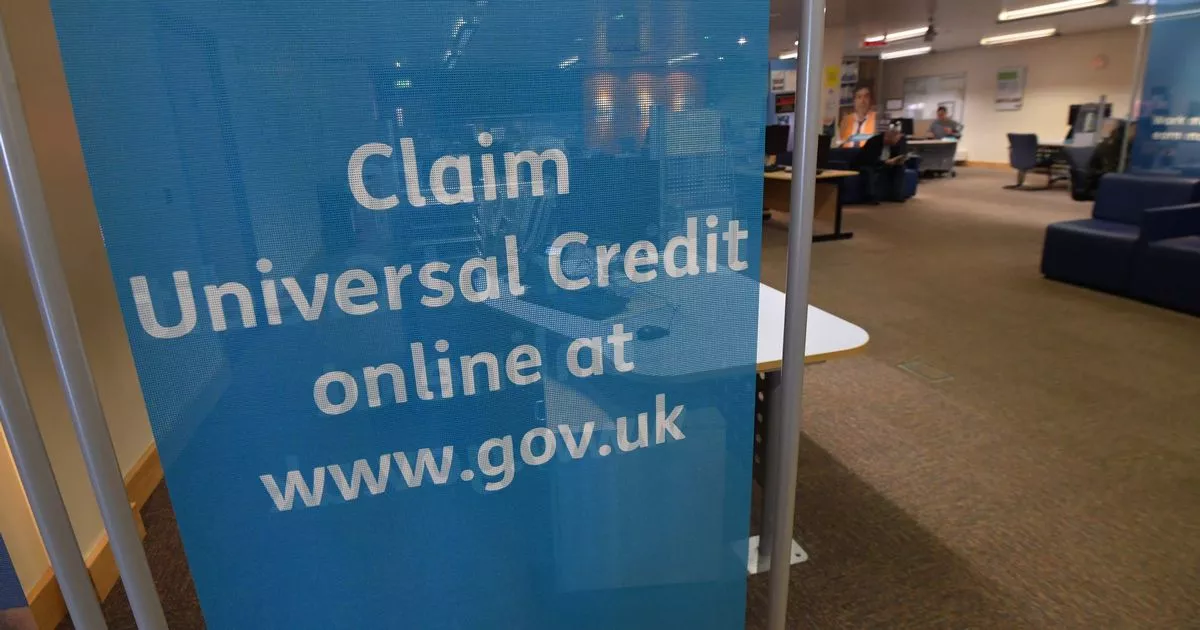
The mechanisms of antifungal resistance are complex and multifaceted, but they generally involve adaptations by the fungus that reduce the effectiveness of antifungal drugs. These mechanisms include: target modification (where the fungal cell alters the target site of the drug), efflux pumps (which actively pump the drug out of the fungal cell), and reduced drug permeability (making it harder for the drug to enter the cell). The rise of antifungal resistance is driven by several factors:
-
Increased use of antifungal drugs in agriculture and medicine: The widespread use of antifungals in agriculture to prevent crop diseases and in medicine to treat human and animal infections has created a selective pressure, favoring the survival and proliferation of resistant strains. The overuse of azoles in agriculture, for example, has contributed significantly to the rise of azole-resistant Aspergillus fumigatus.
-
Overuse and misuse of antifungals: Improper use of antifungals, such as incomplete courses of treatment or the use of broad-spectrum antifungals when narrower-spectrum agents would suffice, accelerates the development and spread of resistance.
-
Lack of new antifungal drug development: The pipeline for new antifungal drugs is alarmingly thin. The high cost and lengthy process of drug development, coupled with limited market incentives, have hampered the introduction of novel antifungal agents.
-
Natural selection leading to resistant strains: Resistant strains naturally arise through random mutations. When exposed to antifungals, these resistant strains have a selective advantage, leading to their dominance within the fungal population.
-
Spread of resistant strains through healthcare settings and the environment: Resistant fungal strains can easily spread through healthcare settings, particularly among immunocompromised patients. They can also persist in the environment, contributing to further dissemination. The emergence of Candida auris, a multi-drug resistant yeast, highlights this critical issue. C. auris is a significant concern due to its high mortality rate and its ability to spread rapidly in healthcare facilities.
Vulnerable Populations and the Severity of Fungal Infections
Fungal infections pose a significant threat to vulnerable populations, whose weakened immune systems are less able to fight off these infections. Individuals at higher risk include:
-
Patients with HIV/AIDS: HIV infection severely compromises the immune system, increasing susceptibility to opportunistic fungal infections.
-
Organ transplant recipients: Immunosuppressive drugs used to prevent organ rejection leave recipients vulnerable to fungal infections.
-
Cancer patients undergoing chemotherapy: Chemotherapy weakens the immune system, making patients susceptible to a range of infections, including fungal infections.
-
Individuals with weakened immune systems due to other diseases: Conditions like diabetes, chronic lung disease, and autoimmune disorders can increase susceptibility to fungal infections.
-
Neonates and infants: Their developing immune systems are not fully equipped to handle fungal infections.
Resistant fungal infections can lead to severe complications, including disseminated disease, organ failure, and death. Mortality rates associated with resistant fungal infections are significantly higher than those with susceptible infections. The prolonged hospital stays and intensive care required for these severe infections result in substantial increases in healthcare costs.
Strategies for Combating Antifungal Resistance
Combating antifungal resistance requires a multi-pronged approach focusing on responsible antifungal use, improved surveillance, and the development of new therapies. Key strategies include:
-
Proper diagnosis and treatment of fungal infections: Accurate and timely diagnosis is crucial to guide appropriate antifungal therapy and prevent the overuse of broad-spectrum antifungals.
-
Strict adherence to prescribed antifungal regimens: Incomplete courses of treatment can lead to the selection of resistant strains.
-
Development and implementation of stewardship programs: Antifungal stewardship programs promote the responsible use of antifungals through education, monitoring, and guideline development.
-
Development of novel antifungal drugs and therapies: Investing in research and development is essential to discover new antifungal agents with novel mechanisms of action, minimizing the risk of cross-resistance. Exploring alternative treatment strategies, such as phage therapy, also holds promise.
-
Improved surveillance and monitoring of antifungal resistance: Surveillance systems are crucial for tracking the emergence and spread of resistant strains, informing infection control practices and guiding treatment decisions.
-
Public health initiatives to promote hygiene and infection control: Improving hygiene and infection control practices in healthcare settings and the community can help reduce the transmission of fungal pathogens.
The Role of Prevention and Hygiene
Preventing fungal infections is crucial in reducing the need for antifungals and slowing the development of resistance. Simple preventative measures can significantly reduce the risk:
-
Hand hygiene: Regular handwashing with soap and water is a simple yet effective way to prevent the spread of fungal pathogens.
-
Proper sanitation: Maintaining a clean and hygienic environment helps reduce the risk of fungal infections.
-
Avoiding exposure to high-risk environments: Avoiding contact with contaminated soil, water, or other environments known to harbor fungal pathogens can minimize exposure risk.
-
Vaccination where available: Although there are limited fungal vaccines currently available, ongoing research may lead to the development of effective vaccines against major fungal pathogens.
Conclusion
The escalating threat of antifungal resistance poses a significant challenge to global health. The lack of new antifungal drugs, coupled with the increasing prevalence of resistant strains, necessitates a multi-faceted approach encompassing responsible antifungal use, enhanced surveillance, and accelerated research into new antifungal agents. Individual responsibility is crucial in combating antifungal resistance. Practice good hygiene, seek prompt medical attention for suspected infections, and support research efforts aimed at developing new antifungal therapies. Learn more about fungal infections and antifungal resistance to become an informed advocate for improved public health strategies. Contact your healthcare provider with concerns regarding fungal infections and consult reputable sources for further information. We must address the growing problem of fungal infections and antifungal resistance before it becomes an insurmountable crisis.
Featured Posts
-
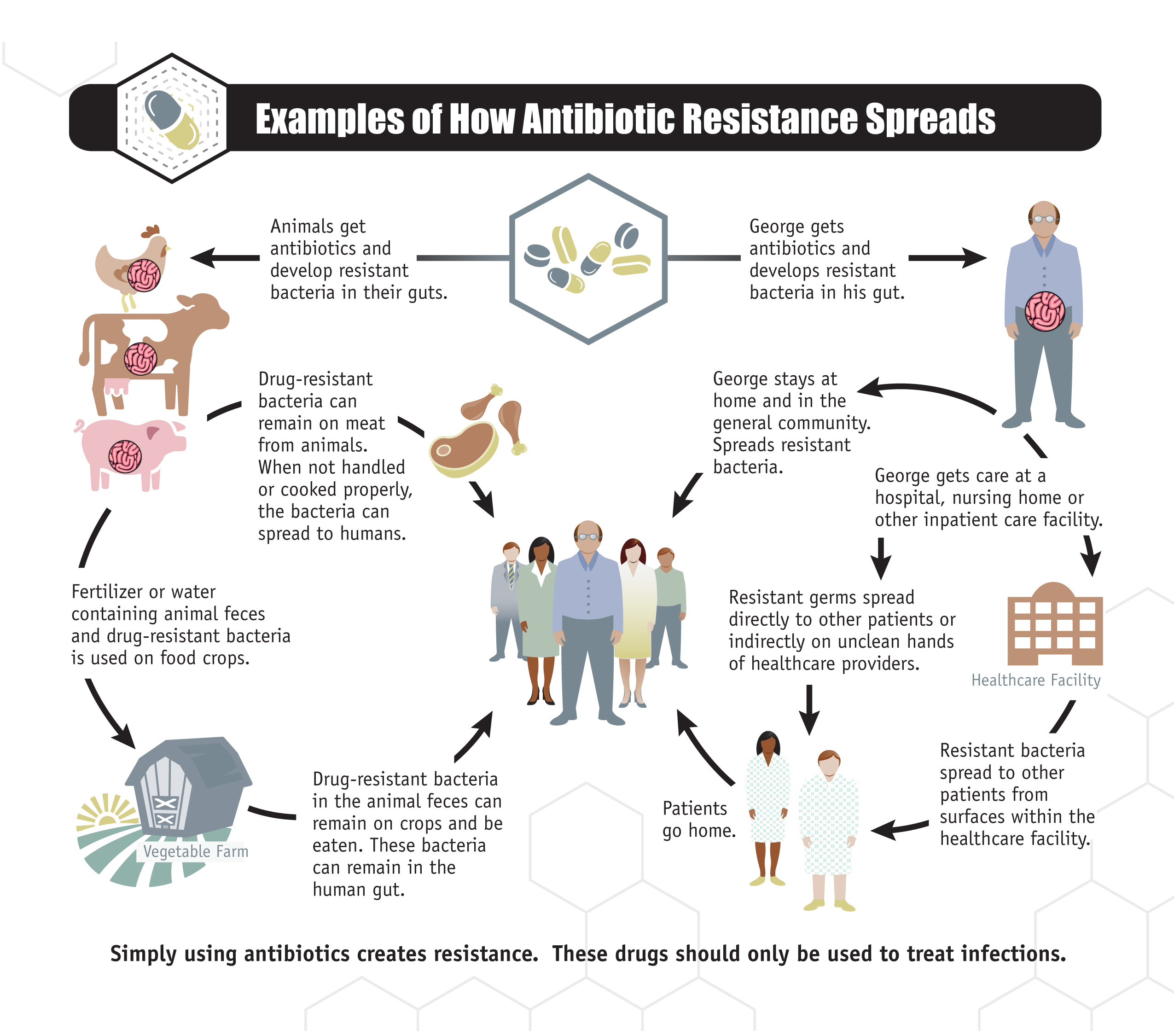
 Navigating The Stock Market In The Shadow Of Liberation Day Tariffs
May 08, 2025
Navigating The Stock Market In The Shadow Of Liberation Day Tariffs
May 08, 2025 -
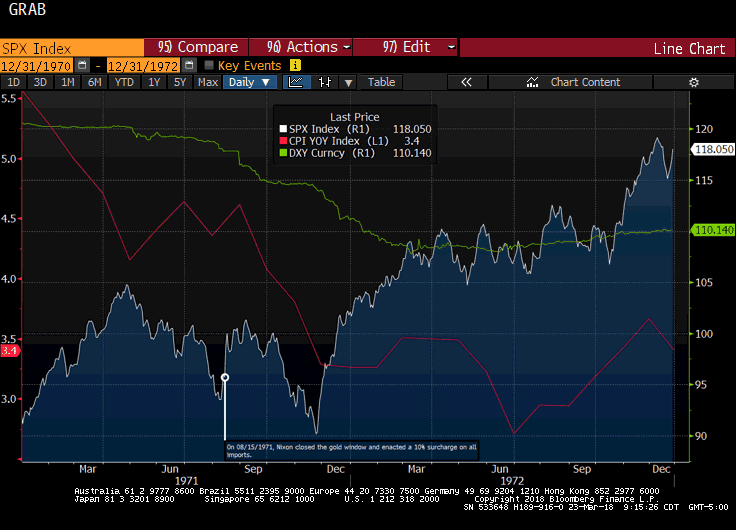
 Dwp Announces Six Month Universal Credit Rule Change
May 08, 2025
Dwp Announces Six Month Universal Credit Rule Change
May 08, 2025 -
 The Hunger Games Directors Stephen King Adaptation A 2025 Horror Release
May 08, 2025
The Hunger Games Directors Stephen King Adaptation A 2025 Horror Release
May 08, 2025 -
 Multidao Se Reune No Vaticano Para O Funeral Do Papa Francisco
May 08, 2025
Multidao Se Reune No Vaticano Para O Funeral Do Papa Francisco
May 08, 2025 -
 Lahwr Ky Edlyh Ke Jjz Ke Lye Nyy Tby Bymh Askym Ka Aelan
May 08, 2025
Lahwr Ky Edlyh Ke Jjz Ke Lye Nyy Tby Bymh Askym Ka Aelan
May 08, 2025
